Precision and Empowerment: Advanced Robotic Surgery in Hoffman Estates at Elite Women’s Care
When it comes to specialized gynecological health, finding advanced robotic surgery in Hoffman Estates is the first step toward a faster recovery and a higher standard of clinical excellence. At Elite Women’s Care, we understand that the decision to undergo surgery is never taken lightly, which is why we prioritize cutting edge technology paired with a deeply compassionate approach. Our facility is dedicated to providing women in Illinois with the most sophisticated surgical options available today, ensuring that every patient feels heard, supported, and confident in their treatment plan.
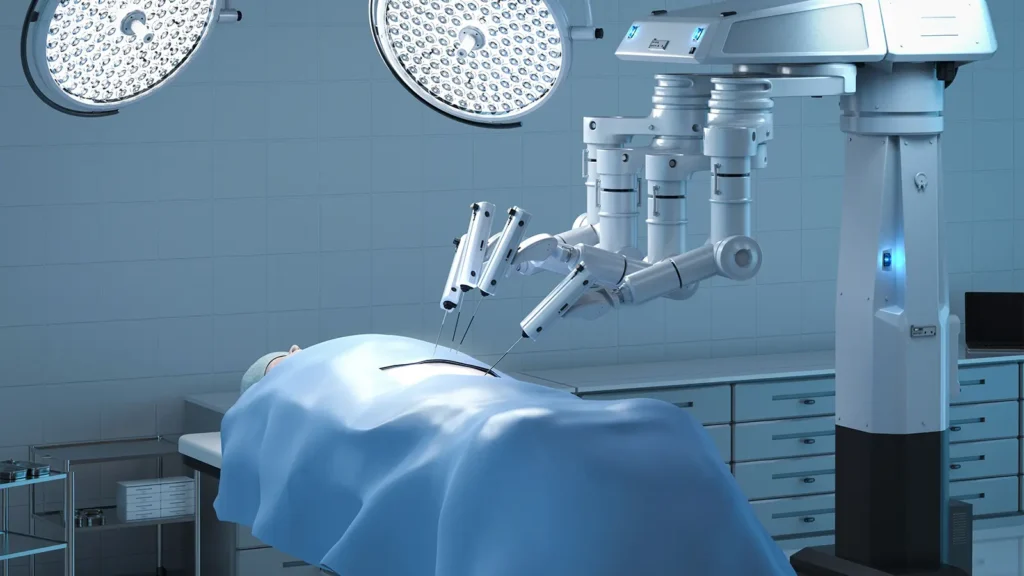
The evolution of surgical technology has transformed the way we approach women’s health, moving away from large incisions and long hospital stays. By choosing robotic surgery in Hoffman Estates, patients gain access to precision guided procedures that were once unimaginable in traditional surgery. This leap forward is not just about the equipment; it is about the empowerment of the patient, offering a path to healing that respects both the physical and emotional needs of women throughout their healthcare journey.
At Elite Women’s Care, our mission is to redefine the surgical experience by blending technical mastery with a patient centered philosophy. Whether you are dealing with chronic pelvic pain, fibroids, or other complex conditions, our team is equipped to provide the highest level of care. We believe that every woman deserves access to the best medical innovations, and our commitment to robotic surgery in Hoffman Estates reflects our dedication to staying at the forefront of the gynecological field.
The Future of Gynecologic Health: da Vinci Surgery Illinois
The cornerstone of our surgical department is the integration of da Vinci surgery Illinois protocols, which utilize a high definition 3D vision system and tiny, wristed instruments. Unlike traditional laparoscopy, this system allows surgeons to operate with enhanced vision, precision, and control. For the patient, this means the surgeon can navigate complex anatomical structures with a level of detail that minimizes impact on surrounding healthy tissue. This technology serves as an extension of the surgeon’s own hands, translating their movements into smaller, more precise actions inside the body.
For women seeking minimally invasive gynecologic surgery, the benefits of this robotic platform are extensive. Because the incisions are significantly smaller than those used in open surgery, patients typically experience much less post operative pain and a reduced need for heavy pain medications. Furthermore, the risk of infection and blood loss is drastically lowered, which is a vital consideration for any major procedure. By choosing da Vinci surgery Illinois, women are often able to return to their daily routines within a fraction of the time required by conventional methods.

Our surgical team at Elite Women’s Care OBGYN is extensively trained in these robotic techniques, ensuring that the technology is utilized to its full potential. We recognize that every patient’s anatomy and medical history are unique, and the flexibility of the robotic platform allows us to tailor each procedure to the specific needs of the individual. This personalized approach to minimally invasive gynecologic surgery is what sets our practice apart, as we focus on achieving the best possible clinical outcomes while prioritizing the patient’s overall well being and comfort.
Specialized Procedures and the Elite Women’s Care Advantage
One of the most common applications for this technology is the robotic assisted hysterectomy, a procedure that has historically required significant downtime. In the past, a hysterectomy often involved a large abdominal incision and a multi day hospital stay. However, with the advancements available at Elite Women’s Care, a robotic assisted hysterectomy allows for a much more refined process. Patients frequently go home the same day or the following morning, experiencing a recovery that is measured in days rather than weeks.
When patients search for the best robotic surgeon near me, they are looking for a combination of experience, success rates, and a bedside manner that puts them at ease. At our Hoffman Estates location, our surgeons are recognized for their expertise in handling complex cases that other practices might deem unsuitable for a minimally invasive approach. Our commitment to robotic surgery in Hoffman Estates means we have the tools to address endometriosis, large fibroids, and pelvic organ prolapse with incredible accuracy, often sparing healthy tissue and preserving nerve function.
The comprehensive care model at Elite Women’s Care OBGYN ensures that the surgical journey is seamless from the initial consultation through the final follow up. We take the time to explain the nuances of minimally invasive gynecologic surgery, answering every question to alleviate any anxiety. Our goal is to ensure that when you choose a robotic assisted hysterectomy or any other robotic procedure, you are doing so with a full understanding of the benefits and the expected recovery timeline.
Key Benefits of Choosing Robotic Assisted Procedures
While the technical aspects are impressive, the real world benefits for our patients are what truly matter. Here are some of the primary reasons women choose our center for their care:
- Enhanced Precision: The robotic system provides a level of steady, filtered movement that exceeds the human hand’s natural capabilities.
- Superior Visualization: Surgeons view the surgical site in 10x magnified, high definition 3D, allowing for better identification of vital structures.
- Reduced Recovery Time: Most patients return to normal activities weeks earlier than those undergoing traditional open surgery.
- Minimal Scarring: Tiny incisions result in scars that are often nearly invisible once fully healed, providing an aesthetic benefit alongside the functional one.
Why Local Expertise Matters for Robotic Care

Navigating the healthcare system can be overwhelming, but finding a top tier Elite Women’s Care OBGYN specialist right here in our community simplifies the process. Accessing robotic surgery in Hoffman Estates means you don’t have to travel far to receive world class medical treatment. Staying local for your surgery and follow up care reduces the stress on both the patient and their family, allowing for a more relaxed environment which is conducive to healing.
If you have been told you need surgery, it is essential to consult with the best robotic surgeon near me to explore all your options. Many patients are surprised to learn that they are candidates for a robotic approach even if they were previously told they needed an “open” procedure. Our specialists at Elite Women’s Care are experts in da Vinci surgery Illinois, and they frequently provide second opinions for women looking to avoid large incisions and long hospitalizations.
The reputation of Elite Women’s Care OBGYN is built on a foundation of trust and successful outcomes. We believe that by offering minimally invasive gynecologic surgery, we are fulfilling a critical need in the community for high tech, high touch medical care. Whether it is a routine procedure or a complex robotic assisted hysterectomy, our focus remains on providing a surgical experience that is as safe, effective, and stress free as possible.
Excellence in Every Incision: Your Journey to Recovery
Choosing the right surgical path is a milestone in your health journey, and selecting robotic surgery in Hoffman Estates places you in the hands of professionals who prioritize your long term vitality. At Elite Women’s Care, we don’t just see a patient; we see a woman with a life, a family, and goals that shouldn’t be sidelined by a long recovery. Our use of da Vinci surgery Illinois technology is a testament to our promise to provide the most advanced care available in the modern medical landscape.
When you are searching for the best robotic surgeon near me, you are looking for a partner in your health who understands the intricacies of the female body. Our team at Elite Women’s Care OBGYN takes great pride in our ability to perform a robotic assisted hysterectomy with such precision that our patients are often amazed at how quickly they feel like themselves again. We are here to guide you through every step, ensuring that your transition from diagnosis to recovery is handled with the utmost professional care and personal empathy.
The future of women’s healthcare is here, and it is defined by the incredible possibilities of minimally invasive gynecologic surgery. We invite you to experience the difference that expert led robotic surgery in Hoffman Estates can make in your life. By combining the latest robotic innovations with a team that truly cares, we ensure that your health is always in the best possible hands.
We are honored to be a leading provider of da Vinci surgery Illinois, helping women reclaim their health and get back to the things they love. At Elite Women’s Care, your wellness is our greatest priority, and our robotic surgical program is designed to deliver the excellence you deserve. Take the first step toward a healthier future by scheduling a consultation with the best robotic surgeon near me and discover how our advanced techniques can transform your surgical experience.